HIV/AIDS
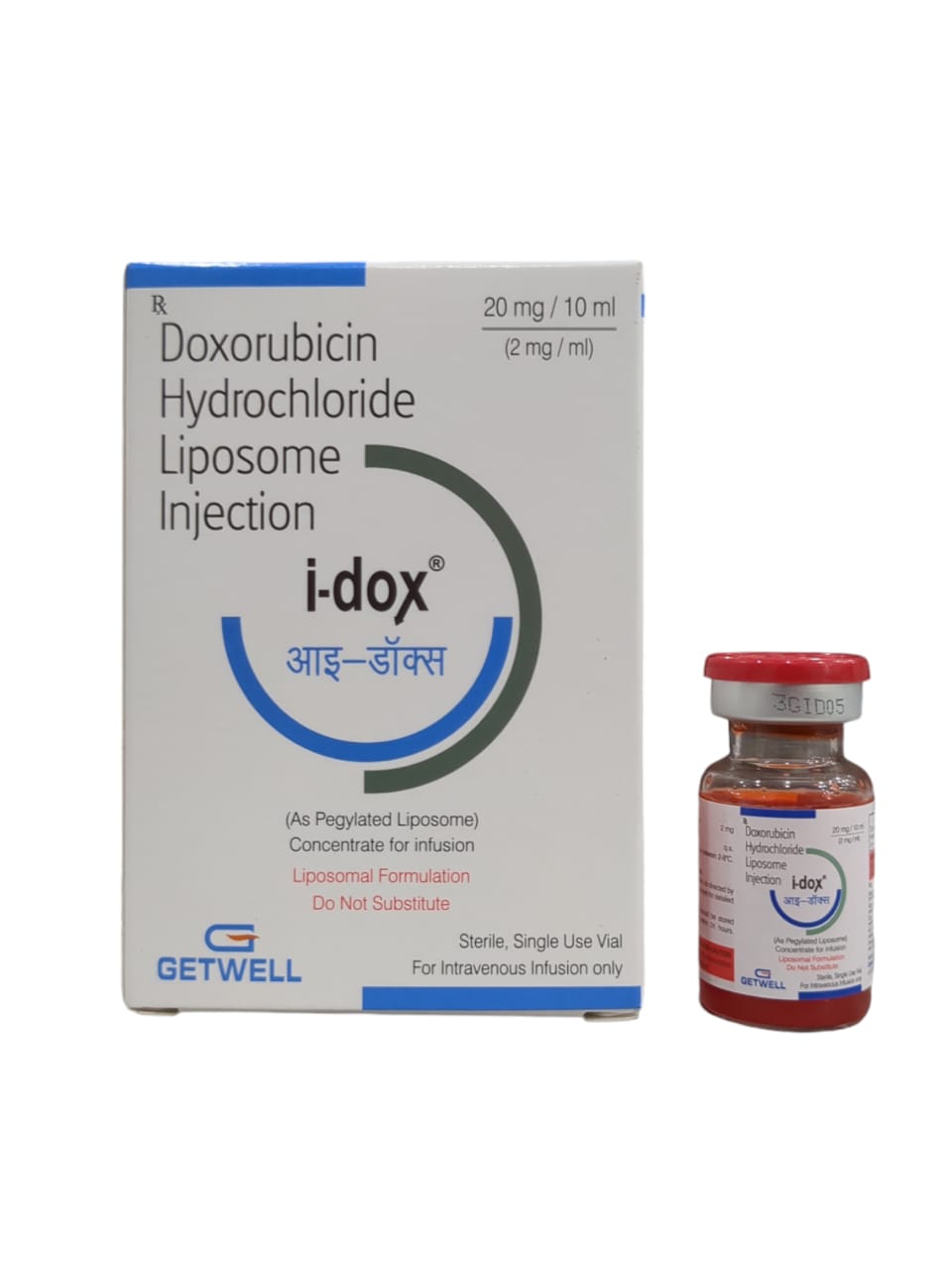
About I-Dox 20Mg/10Ml Inj
I-Dox 20Mg/10Ml Inj is an anti-cancer medicine used in the treatment of cancer. Cancer is a disease where the cells grow abnormally and divide uncontrollably. I-Dox 20Mg/10Ml Inj is primarily used as adjuvant chemotherapy in women with axillary lymph nodes with involvement resection of breast cancer (abnormal growth in the cells of the breast). It is also used to treat neuroblastoma (cancer that starts in nerve cells and primarily affects children) and Wilms' tumor (a form of kidney cancer that affects children).
I-Dox 20Mg/10Ml Inj contains Doxorubicin, which belongs to the class of anthracycline topoisomerase inhibitors. It inhibits the topoisomerase II enzyme by intercalating the DNA base pairs. This causes double helix DNA to be uncoiled, destroying DNA and RNA synthesis.
I-Dox 20Mg/10Ml Inj may cause certain side effects such as nausea, headache, abdominal pain, loss of appetite, vomiting, dizziness, mouth sores, tiredness, back pain, red discoloration of urine, diarrhea, and pain at the site of injection. Most of these side effects do not require medical attention and gradually resolve over time. However, if the side effects persist, please consult your doctor. A trained healthcare doctor will administer I-Dox 20Mg/10Ml Inj. So, do not self-administer. Your doctor will decide the dose of the medicine based on your health condition.
I-Dox 20Mg/10Ml Inj should be avoided if you are allergic to it or any other components of this medicine. It is contraindicated in patients having severe myocardial insufficiency, a recent history of myocardial infarction (MI), severe persistent drug-induced myelosuppression, and severe liver disease. Hence, if you have any such conditions, inform your doctor. Inform your doctor if you have any cardiovascular conditions, liver/kidney disease, or taking any CYP3A4 or CYP2D6 inducers medication, as it can cause adverse effects. I-Dox 20Mg/10Ml Inj is known to cause embryo-fetal toxicity. Hence, if you are pregnant or breastfeeding, inform your doctor beforehand.
Uses of I-Dox 20Mg/10Ml Inj
Treatment of Breast Cancer
Directions for Use
A trained healthcare professional will administer I-Dox 20Mg/10Ml Inj. Hence, do not self-administer.
Medicinal Benefits
I-Dox 20Mg/10Ml Inj contains Doxorubicin, which belongs to the class of anthracycline topoisomerase inhibitors. It inhibits the topoisomerase II enzyme by intercalating the DNA base pairs. This causes double helix DNA to be uncoiled, thereby destroying the DNA and RNA synthesis. I-Dox 20Mg/10Ml Inj is also used in the treatment of acute lymphoblastic leukaemia, acute myeloblastic leukaemia, Hodgkin lymphoma, Non-Hodgkin lymphoma, metastatic breast cancer, metastatic Wilms’ tumour, metastatic neuroblastoma, metastatic soft tissue sarcoma, metastatic bone sarcomas, metastatic ovarian carcinoma, metastatic transitional cell bladder carcinoma, metastatic thyroid carcinoma, metastatic gastric carcinoma, metastatic bronchogenic carcinoma.
How I-Dox 20Mg/10Ml Inj Works
I-Dox 20Mg/10Ml Inj contains Doxorubicin, which belongs to the class of anthracycline topoisomerase inhibitors. It inhibits the topoisomerase II enzyme by intercalating the DNA base pairs. This causes double helix DNA to be uncoiled, destroying DNA and RNA synthesis.
Storage
Store in a cool and dry place away from sunlight
Side Effects of I-Dox 20Mg/10Ml Inj
Nausea
Abdominal pain
Vomiting
Dizziness
Back pain
Pain at the site of injection
Red discolouration of urine
Loss of appetite
Mouth sores
Tiredness
Weight gain
What if I have taken an overdose of I-Dox 20Mg/10Ml Inj
Since I-Dox 20Mg/10Ml Inj is given in a controlled medical setting by a healthcare professional, an overdose is not likely to occur. If you think there has been an overdose or experiencing any adverse events, get medical care right away. In a medical setting, an overdose would be treated quickly. Overdose of I-Dox 20Mg/10Ml Inj may cause sores in the mouth and throat, fever, sore throat, chills, or other signs of infection, unusual bleeding or bruising, black and tarry stools, red blood in stools, and bloody vomit or vomited material that looks like coffee grounds.
Drug Warnings
I-Dox 20Mg/10Ml Inj should be avoided if you are allergic to it. It is contraindicated in patients having severe myocardial insufficiency, a recent history of myocardial infarction (MI), severe persistent drug-induced myelosuppression and severe liver disease. Hence avoid using this medicine under such conditions. Inform your doctor if you have any cardiovascular conditions, liver/kidney disease, or taking any CYP3A4 or CYP2D6 inducers medication, as it can cause serious adverse effects. I-Dox 20Mg/10Ml Inj is known to cause embryo-fetal toxicity. Hence it is contraindicated in pregnant or breastfeeding women. Do not stop receiving I-Dox 20Mg/10Ml Inj without a doctor’s advice, as it can cause serious health conditions. I-Dox 20Mg/10Ml Inj is known to cause secondary malignancies.
Send
Message